Information on infection Rate _ please read the article! It is from Feb 18 - newer material should be coming soon.
These 2 questions will determine if the coronavirus becomes a deadly pandemic
We still don’t have firm answers to the most important questions about this virus.
By
Julia Belluz@juliaoftorontojulia.belluz@voxmedia.com Feb 18, 2020, 10:50am EST ps://www.vox.com/2020/2/18/21142009/coronavirus-covid19-china-wuhan-deaths-pandemic
Seven weeks into the outbreak of the new coronavirus, we’re still far from answering an urgent question: Will this become a deadly pandemic that sweeps around the world?
Since China first announced the outbreak on December 31,
73,336 cases have been recorded, including 1,875 deaths.
While the vast majority of cases and deaths are still occurring in mainland China, Covid-19 has already made its way to
at least 25 other countries, including the US, Malaysia, Egypt, and Canada.
Markets are on edge.
Businesses and
cruise ship itineraries have been interrupted. Cities and countries are responding with
unprecedented quarantines and
travel bans. The whole thing feels a lot like the 2011 pandemic film
Contagion.
But to know whether this is really the next deadly
pandemic — a disease that
spreads globally and could kill millions of people — we need answers to two basic questions: How easily does Covid-19 spread from person to person, and how severe is the virus? At the moment, scientists only have informed guesses, which are likely to solidify in the coming weeks and months. But they’re learning more by the day — and what we know so far is instructive.
The R0, explained
With every disease outbreak, epidemiologists try to figure out how far — and how fast — a virus is likely to spread through a population. To do that, they use the
basic reproduction number, called the “R naught,” or R0.
The figure refers to how many other people one sick person is likely to infect on average in a group that’s susceptible to the disease (meaning they don’t already have immunity from a vaccine or from fighting off the disease before).
The R0 is super important in the context of public health because it foretells how big an outbreak will be. The higher the number, the greater likelihood a lot of people will fall sick.
Measles, the most contagious virus researchers know about, can linger in the air of a room and sicken people up to two hours after an infected person who coughed or sneezed there has left. If people exposed to the virus aren’t vaccinated, measles’ R0 can be as high as 18.
Ebola is more deadly but much less efficient: Its R0 is typically just 2, in part, because many infected individuals die before they can pass the virus to someone else.
Related
A SARS-like virus is spreading quickly. Here’s what you need to know.
Now, here’s a big caveat: The R0 is not “something that is fixed,” said Marion Koopmans, who studies emerging infectious diseases and heads the department of virology at the Erasmus Medical Center in Rotterdam, Netherlands.
That’s because diseases behave differently in different environments, depending on factors like population density and susceptibility to a disease in a population. For example, in the case of norovirus — that nasty and highly contagious bug infamous for causing outbreaks of stomach flu on
cruise ships — the R0 estimates vary depending on whether the outbreak is contained in one place (like a hospital) or spread more widely.
Some individuals are also more contagious — and have a higher R0 — than others, because of their viral load, for example, or the airflow in the building where they’re sick. (The folks who are especially contagious are known as “
super-spreaders.”)Diseases can also spread more easily in places with a weak public health system.
What we know about how easily the new coronavirus spreads
With these caveats in mind, here’s what we know about the R0 for the new coronavirus.
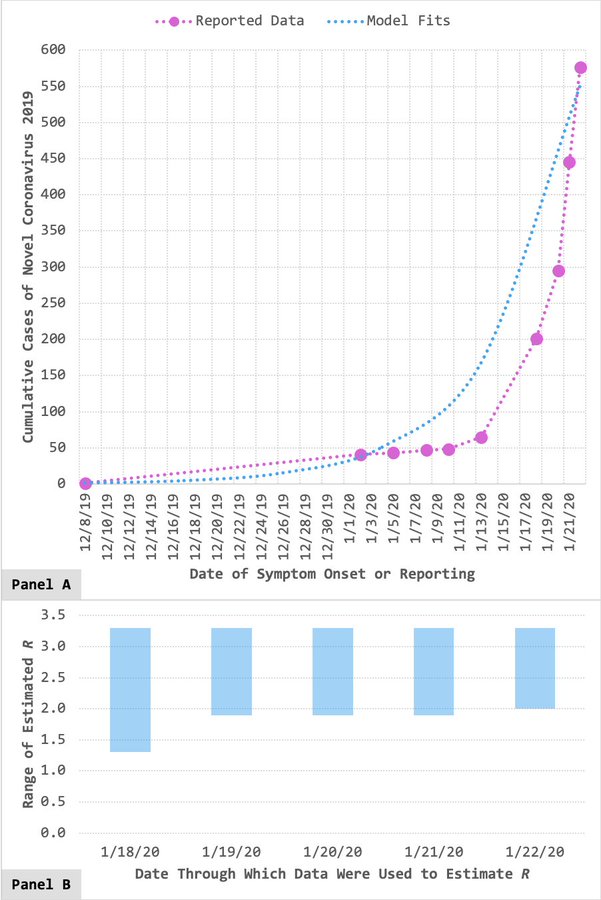
There are literally dozens of estimates about Covid-19’s R0 floating around, from research groups around the world. And different research groups use different statistical models, assumptions, and data to plug into their models. According to a World Health Organization spokesperson, Tarik Jašarević, as of February 17, the estimates of R0 spread are uniformly above 1 (meaning the virus is sustaining itself among humans), and most settle around 2 to 2.5 (meaning each infected person is causing two or 2.5 others to become infected).
If one narrows the estimates to some of the world’s top epidemiological modeling labs — like
Maia Majumder’s at Boston Children’s Hospital or
Christian Althaus’s at the University of Bern or
Jon Read’s at Lancaster or
China CDC’s — the range looks a little broader: 2 to
3.11. That would make the new coronavirus more contagious than seasonal flu and potentially even more contagious than SARS.
“Given the recent emergence of this disease, the very limited data available, and the very different methods employed for estimation, the consistency of these estimates is remarkable,” Toronto epidemiologist
David Fisman told Vox in an email.
Still, it’s early days. “It’s difficult or impossible to get an accurate R0 at the beginning of an epidemic,” said Daniel Lucey, an infectious diseases physician and adjunct professor of infectious diseases at Georgetown University Medical Center. We don’t yet
know exactly when or how the outbreak began, where it’s spread, or how many people are sick. Only in the coming weeks — as researchers gather more data on how the virus is moving — will they be able to refine the R0. And, again, it’ll likely look different in low-income countries in Africa than it will in high-income countries like the US or Canada.
Related
For now, though, there are a couple of things they can say. “Because it’s above 1, that means we know it can cause sustained transmission in humans,” said Maia Majumder, faculty at Boston Children’s Hospital’s Computational Health Informatics Program. An R0 below 1 means an outbreak is likely to burn out. But, “Just because the number is high [like SARS’s R0 or the upper end of the current Covid-19 estimate] doesn’t mean it’s going to cause a massive pandemic.”
“We do have good examples of high reproductive number diseases like SARS,” Majumder added. “It had no vaccine, no specific care approach, and we still managed to get the situation under control.” That’s because the R0 can’t account for all the interventions public health officials put in place, like antivirals or infection control measures in hospitals.
Plus, Jašarević, the WHO spokesperson said, “how quickly a virus spreads is not linked to how sick it can make people. Though Covid-19 may spread more easily than SARS, it is not as deadly. That said, it still has the potential to make many people sick and to kill some, and thus containing or managing its impact are global priorities.” So let’s turn to what we know about Covid-19’s deadliness.
What we know about how deadly the coronavirus is
Next to the R0, the other most important way to understand how bad an outbreak could get is the
case fatality rate, or CFR. In simple terms, it’s the proportion of deaths a disease causes within a group of people who have the disease.
Here, too, there are problems with arriving at a solid estimate at the moment. To have a firm understanding of the CFR, you need to know how many people in a population have the virus, and among those, how many die.And early on in outbreaks, we don’t often know.
That’s because the sickest are usually the ones who show up at doctor’s offices and in hospitals. But there may be hundreds or thousands of others with the virus who never show symptoms, or never bother going to see a doctor because they’re not very sick. (That’s why the CFR can often look much worse in the early days of an outbreak.)
Getting an accurate CFR would require a survey of the Chinese population to find out who has antibodies for the virus, said Majumder, including the folks who didn’t even know they had it. That’ll give experts the denominator — the real case toll — in the CFR equation. “Until we’ve done [that] — and I’m sure it’ll happen sometime in the future — there are going to be some people that have mild infections or are asymptomatic infections that we’re not picking up.”
And as it stands, we don’t yet have the
serology test we’d need to do this type of testing. Plus, since the virus has an incubation period of up to two weeks, there are many people with the infection in limbo or still in hospitals, who may or may not survive the pneumonia that comes with it.
So while there’s a great hunger for clarity about how bad the outbreak will become, frustratingly at this stage, researchers need time to work that out.
In the meantime, we have some preliminary estimates we can look to. On February 16,
China’s CDC published a report of the first 72,314 patients with confirmed or suspected Covid-19 in mainland China. It’s the largest such analysis to date. And it found an overall CFR of 2.3 — suggesting Covid-19 is less deadly than SARS, which had a CFR of around 10 percent.
They also found a huge variation in the case fatality rate by age group. In short, the CFR goes up with each passing decade. You can see the trend in this table from the study — the CFR rises from 0.2 in people ages 10 to 19 to 1.3 in 50-year-olds to 14.8 in those who are 80-plus:
:no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/19726923/Screen_Shot_2020_02_18_at_9.09.31_AM.png)
Case fatality rates in mainland China as of February 11, 2020.
China CDC One major caveat here: This data comes from mainland China, where all but six of the 1,875 deaths have occurred. And for reasons no one understands,
the case fatality rate has been lower outside of mainland China.
But, again, it’ll be a while before we know the true number of cases and have a better understanding of the deaths.
Here is what we know for sure: While nearly 2,000 people have died in this outbreak so far, seasonal flu kills between 250,000 and 650,000 people annually. For most people, “you’re probably more likely to be catching flu than you are to be getting coronavirus,” said Devi Sridhar, chair in global public health at the University of Edinburgh.
:format(webp):no_upscale()/cdn.vox-cdn.com/uploads/chorus_asset/file/19733807/Artboard_6_80.jpg)
We've updated our transmissibility assessment for
#nCoV2019! R_0 estimates (based off of publicly reported confirmed cases through 1/26/20 & subject to change) remain ~stable, now ranging from 2.0 to 3.1.
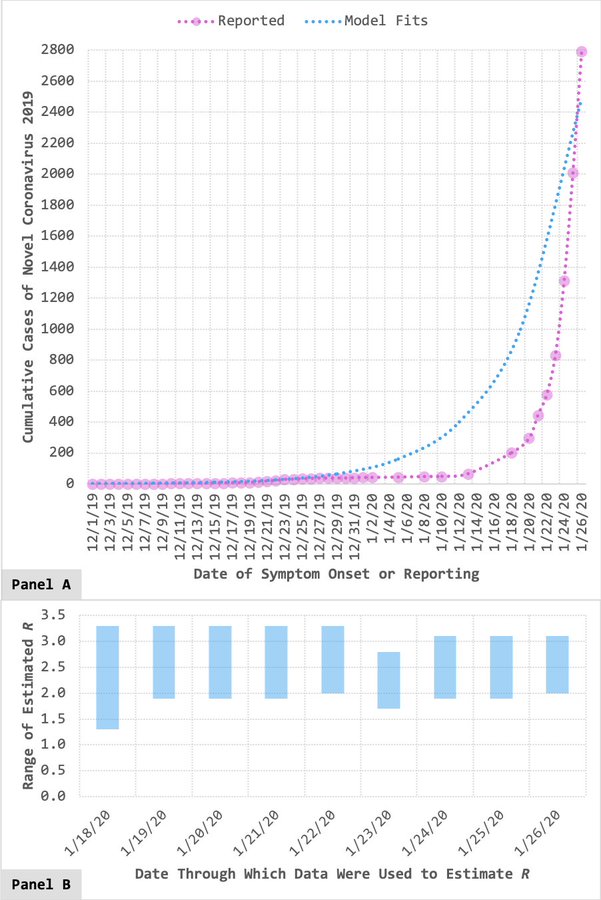
if we assume the R0 of Wuhan coronavirus is around 2-3 - meaning for each infected person - 2-3 other people will be infected and a case mortality rate of likely less than 0.1% - We have a snapshot of the disease impact. The above case fatality rates are from very early numbers out of Chin, primarily - and better information is developing.
FYI!
Now - what nonsense will the resident fireman and other assorted DPST "experts" have to offer - Trump hate and Trump is responsible for having the American military plant the virus in Wuhan!